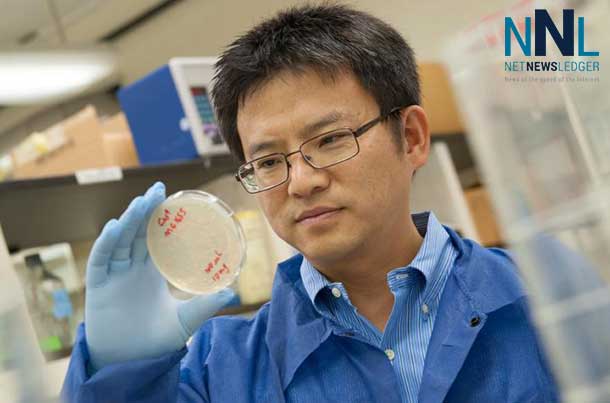
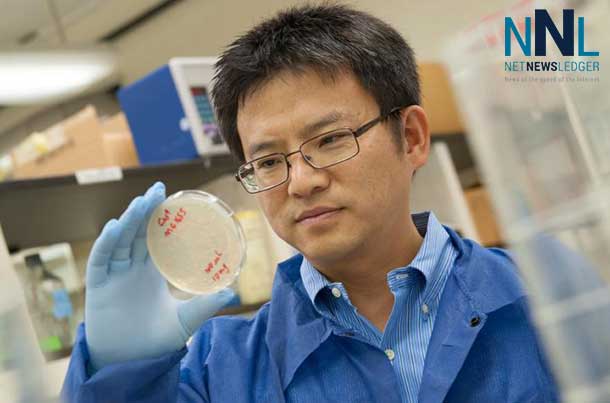
Credit: Nick Romanenko/Rutgers University
THUNDER BAY – HEALTH – Type 2 diabetes affects an estimated 28 million Americans according to the American Diabetes Association, but medications now available only treat symptoms, not the root cause of the disease. New research from Rutgers shows promising evidence that a modified form of a different drug, niclosamide – now used to eliminate intestinal parasites – may hold the key to battling the disease at its source.
Across Northwestern and Northern Ontario, diabetes is a major cause of health problems and death.
The study, led by Victor Shengkan Jin, an associate professor of pharmacology at Rutgers Robert Wood Johnson Medical School, has been published online by the journal Nature Medicine.
Jin says it is important to find a suitable medication to correct the cause of the disease as quickly as possible because the only way now known to “cure” the disease involves major gastric bypass surgery. “The surgery can only be performed on highly obese people,” Jin explains, “and carries significant risks that include death, so it is not a realistic solution for most patients.”
And the number of patients continues to rise. The Centers for Disease Control and Prevention projects that 40 percent of all Americans now alive will develop type 2 diabetes.
Type 2 is the form of diabetes once known as “adult onset,” in which the body produces insulin that ordinarily would keep blood sugar under control, but either it does not produce enough insulin or the body’s ability to use that insulin is degraded.
According to Jin, a major cause of insulin resistance is the accumulation of excess fat in the cells of the liver, as well as in muscle tissue. The fat disrupts the process where, ordinarily, insulin would cause body tissues to correctly absorb glucose – blood sugar – and use it as a fuel. With nowhere else to go, much of the excess glucose remains in the bloodstream, where in high concentrations it can damage tissues throughout the body – potentially leading to blindness, kidney damage, cardiovascular diseases and other severe health problems.
“Our goal in this study was to find a safe and practical way of diminishing fat content in the liver. We used mice to perform proof-of-principle experiments in our laboratory,” says Jin. “We succeeded in removing fat, and that in turn improved the animals’ ability to use insulin correctly and reduce blood sugar.”
The modified medication – whose full name is niclosamide ethanolamine salt (NEN) – burned the excess fat in liver cells through a process known as mitochondrial uncoupling. Mitochondria are the microscopic energy source for each cell in the body, and ordinarily – like a well-tuned car engine – they burn fuels including fats and sugars in modest quantities to keep the cells functioning.
“The cell is like a car and the mitochondria are the engine,” Jin explains. “What we’re doing inside cells is like putting the car’s transmission into neutral by uncoupling it from the transmission. Then you step on the gas so the engine runs full throttle but the car doesn’t move. If too much of the fuel in the cell is fat, you keep burning it until the fuel gauge reaches empty. Without the interference of fat, you hope that sugar will then enter the cell normally.”
Getting rid of the interference of fat in liver and muscle tissue is the key to restoring the cells’ ability to respond to insulin properly, which would allow the right amount of sugar to be taken up by cells and ultimately reverse the diabetes entirely. That outcome is far from certain, but Jin says the positive changes he saw in the mice are encouraging.
Jin says it also is significant that the drug he used is a modified form of a medication that the FDA already approved for human use. That was a deliberate choice. “We wanted a safe and practical compound to deplete fat inside cells,” says Jin. “We went to the literature and found an approved drug that does in parasitic worms what we wanted to do in liver cells. The modified form of the medication, although itself is not a drug used in humans, has an excellent safety profile in other mammals – so very likely it would have a good safety profile in humans too.”
Also, excess fat in the liver is not just a condition of the obese; people of normal weight can develop fatty livers and type 2 diabetes. Jin says this kind of medication, if shown to be effective, could safely treat patients of all weights.
Jin is cofounder of a company called Mito BioPharm, established in 2012, which has the exclusive right to use a patent owned by Rutgers to develop NEN for potential commercial use.







