THUNDER BAY – Health News – Why is it that after a stroke, some patients recover faster and better than others? And are there ways we can help that process?
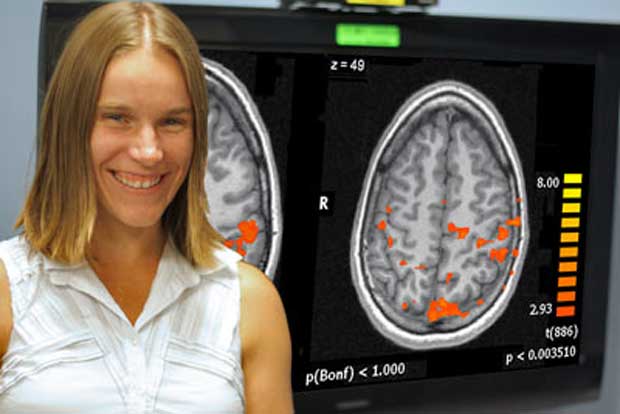
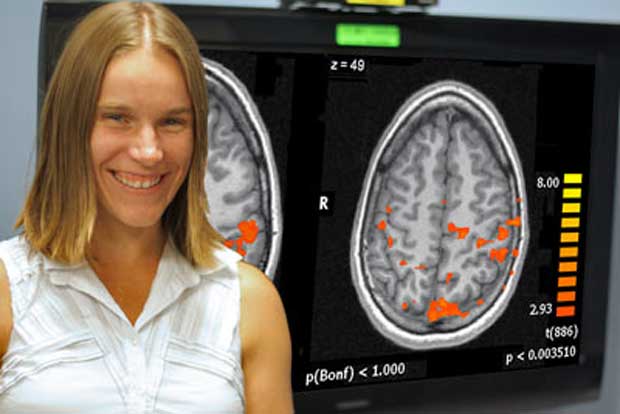
Those are two of the questions that Dr. Jane Lawrence-Dewar of the Thunder Bay Regional Research Institute (TBRRI) will be investigating shortly. At first, her research will concentrate on hand coordination, how that coordination is affected by stroke, and how it recovers or adapts after stroke.
“We know that following a stroke injury, many patients can recover some hand function, but that amount is always variable,” Dr. Lawrence-Dewar said. “We really just don’t know what is happening in the brain in order to make that happen.”
Generally speaking, the brain is often able to “re-map” itself after an injury, creating new pathways around the injured area. But this happens differently in each patient.
“I’m interested in what changes in the patterns of brain activity in order to facilitate that recovery.”
Dr. Lawrence-Dewar uses a method called functional Magnetic Resonance Imaging or fMRI. This method detects brain activity based on changes in blood flow and blood oxygenation. It is a non-invasive technique that doesn’t require a contrast or radiation.
The study itself will measure the brain activity of a stroke patient while they are simply lying down inside the MRI. Then, the patient will be asked to do some sort of task, at which point certain areas of the brain will light up.
“What I aim to do is try to piece together the differences in the patterns laid out when people recover well versus when they aren’t as well,” she said. “If we can learn what areas of the brain we need to get active, perhaps we can use that knowledge in order to make our rehab methods more effective or develop new tools that can better target that re-mapping.”
What makes the research even more complex is that every stroke patient will be different, both in injury and recovery.
“This is one of the challenges – and one of the arguments for having techniques that enable personalized medicine,” Dr. Lawrence-Dewar said.
In other words, once you are able to study the patient’s particular injury and get insight based on previous cases to see what treatment approach might work best, doctors can create a rehab routine that is custom-made for that patient.
Right now, Dr. Lawrence-Dewar is waiting for additional equipment, including a projection screen and a specialized all-plastic trackball that can safely enter the MRI unit with the patient (steel and other metals are not allowed within the strong magnetic field) so the patient can see and react to events on the screen. These tools will help her determine hand function while simultaneously observing fMRI images of the brain to see which areas are lighting up – and which aren’t.
The current project will take about two years to complete, Dr. Lawrence-Dewar said, though she expects it will evolve into other areas of study. This research will provide a scientific “baseline” for future studies that could investigate ways of helping patients improve recovery by assisting with the brain re-mapping in some way.
“Right now I’m at Step 1,” Dr. Lawrence-Dewar said.